Finding blood in your urine after taking Lasix (furosemide) warrants immediate attention. This isn’t always a cause for alarm, but it requires prompt medical evaluation. While Lasix is a powerful diuretic, it can sometimes irritate the urinary tract, potentially leading to microscopic hematuria (blood not visible to the naked eye) or, less commonly, macroscopic hematuria (visible blood).
The presence of blood can stem from several factors. Lasix’s effect on blood volume and pressure can impact the delicate capillaries in your kidneys, causing minor bleeding. Pre-existing kidney conditions might also be exacerbated by Lasix, increasing the likelihood of blood in the urine. It’s crucial to discuss your complete medical history with your doctor, including any pre-existing kidney issues, or conditions such as urinary tract infections (UTIs) or kidney stones, as these can interact with Lasix.
Do not self-treat. Contact your doctor or healthcare provider immediately if you notice blood in your urine after taking Lasix. They will conduct a thorough assessment, possibly including urine tests, to determine the cause and advise on the appropriate course of action. This may involve adjusting your Lasix dosage, modifying your treatment plan, or investigating underlying medical issues.
Remember: This information serves for educational purposes only and does not substitute professional medical advice. Always consult with your doctor before making any changes to your medication regimen.
- Lasix and Blood in Urine: Understanding the Connection
- How Lasix Affects Your Kidneys
- Other Factors Contributing to Hematuria
- When to Seek Medical Attention
- Risk Factors & Management
- Consult Your Doctor
- Note: This information is for educational purposes only and does not constitute medical advice. Always consult your physician for any health concerns.
- Lasix’s Mechanism and Potential for Hematuria
- Identifying Blood in Urine: Symptoms and Diagnosis
- Diagnosis of Hematuria
- Additional diagnostic tests
- When to Seek Medical Attention: Risk Factors and Complications
- Managing Lasix-Related Hematuria: Treatment and Prevention
Lasix and Blood in Urine: Understanding the Connection
Lasix, a powerful diuretic, can sometimes cause blood in your urine (hematuria). This isn’t always a cause for immediate alarm, but it requires attention. The connection lies primarily in Lasix’s mechanism of action.
How Lasix Affects Your Kidneys
Lasix increases urine production by blocking the reabsorption of sodium and water in your kidneys. This increased flow can sometimes irritate the delicate tissues lining your urinary tract, leading to microscopic bleeding. This often presents as a pinkish or reddish tinge in your urine, although significant bleeding is less common.
Other Factors Contributing to Hematuria
Pre-existing kidney conditions, such as kidney stones or infections, can increase the risk of Lasix-related hematuria. Similarly, dehydration, which can be aggravated by Lasix if not properly managed, can also contribute.
When to Seek Medical Attention
While minor, temporary blood in the urine after starting Lasix might be normal, significant bleeding or persistent hematuria warrants immediate medical evaluation. Pay close attention to the color and amount of blood in your urine. Dark red or brown urine indicates more serious bleeding.
Risk Factors & Management
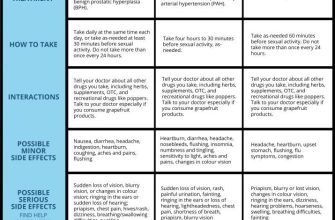
| Risk Factor | Management Strategy |
|---|---|
| Pre-existing kidney disease | Close monitoring of kidney function, possibly adjusting Lasix dosage. |
| Dehydration | Increase fluid intake, potentially altering Lasix dosage or administration schedule. |
| Urinary tract infections | Prompt treatment of infections as prescribed by your physician. |
Consult Your Doctor
Always discuss any changes in your urine, including the presence of blood, with your doctor. They can properly assess the situation, determine the cause, and adjust your treatment plan accordingly. They might also perform tests to rule out other potential issues.
Note: This information is for educational purposes only and does not constitute medical advice. Always consult your physician for any health concerns.
Lasix’s Mechanism and Potential for Hematuria
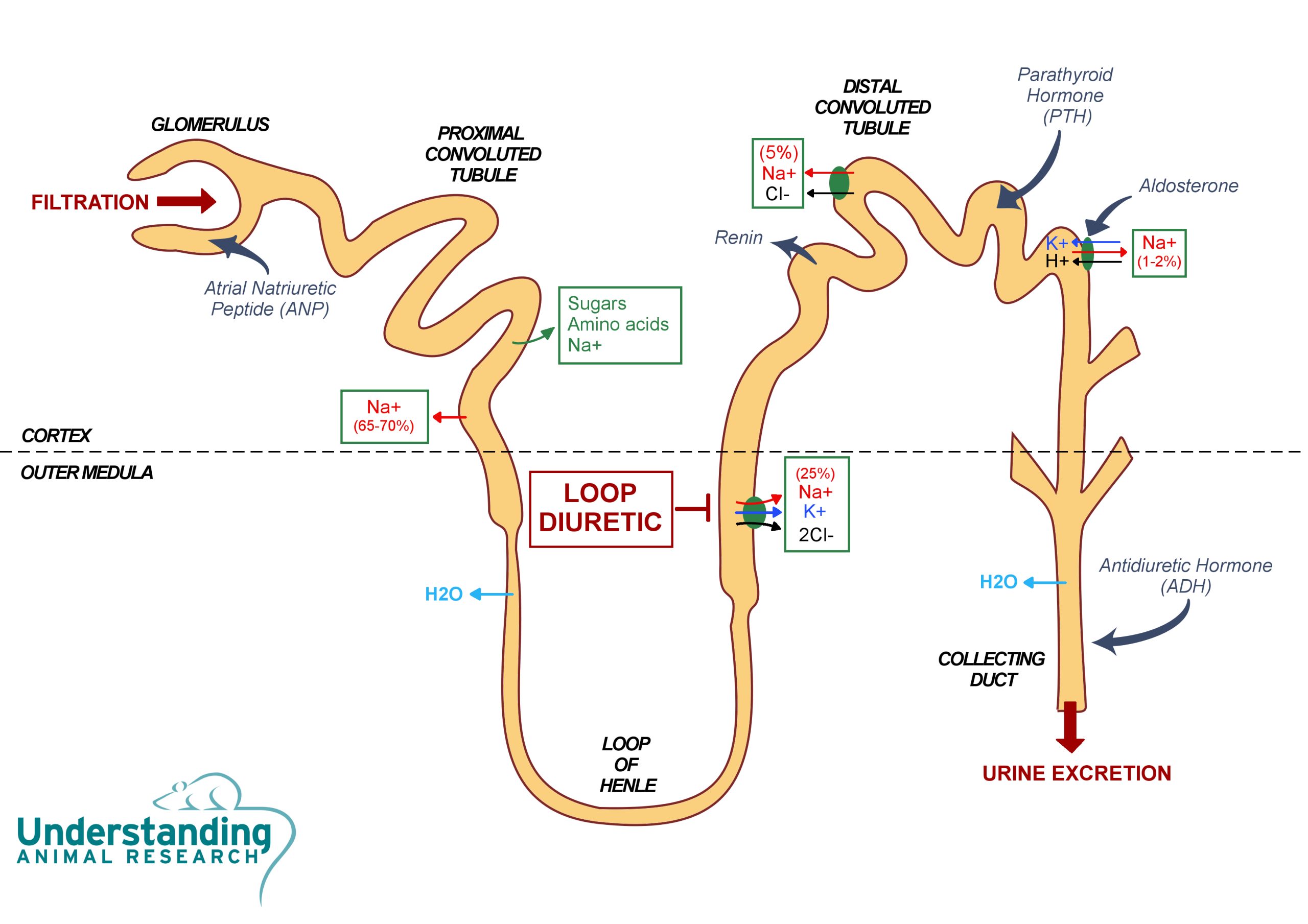
Lasix, or furosemide, powerfully increases urine output by blocking sodium and chloride reabsorption in the loop of Henle. This leads to increased water excretion. However, this diuretic effect can sometimes contribute to hematuria (blood in the urine).
Here’s how it might happen:
- Increased Urine Flow Rate: Higher urine flow rates can irritate the urinary tract, potentially causing microscopic bleeding. This is more likely in individuals with pre-existing urinary tract conditions.
- Dehydration: While Lasix increases urine output, excessive diuresis can lead to dehydration. Dehydration concentrates the urine, potentially causing irritation and microscopic bleeding.
- Pre-existing Renal Conditions: Patients with underlying kidney problems may experience exacerbated bleeding due to the increased pressure and stress on the kidneys from the diuretic effects of Lasix.
- Drug Interactions: Some medications, when taken concurrently with Lasix, can increase the risk of bleeding. Always inform your doctor of all medications you are taking.
Recognizing hematuria as a potential side effect is key. Noticeable blood in your urine requires immediate medical attention.
Recommendations:
- Hydration: Maintain adequate hydration to counter the dehydrating effects of Lasix. Always follow your doctor’s prescribed dosage and instructions.
- Regular Monitoring: Routine urinalysis can help detect early signs of hematuria, allowing for timely intervention.
- Transparency with Your Doctor: Report any changes in urine color or volume immediately to your physician.
This information should not replace professional medical advice. Consult your physician for diagnosis and treatment.
Identifying Blood in Urine: Symptoms and Diagnosis
Notice blood in your urine? It can appear bright red, cola-colored, or even go unnoticed until a urine test reveals it. This condition, hematuria, often manifests with no other symptoms. However, pain during urination (dysuria) or increased urinary frequency might accompany it. The color change is the most noticeable sign. If you see blood in your urine, seek medical attention immediately.
Diagnosis of Hematuria
Your doctor will start with a thorough medical history and physical exam. They’ll ask about your symptoms, medications, and any relevant family history. A urinalysis is the first diagnostic test. This simple test examines the urine’s physical properties, checks for infection, and identifies the presence of blood cells. Microscopic analysis can reveal the number and type of red blood cells. A urine culture helps rule out urinary tract infections, a common cause of blood in urine. Further investigations, like a cystoscopy (camera inserted into the bladder) or imaging tests (ultrasound, CT scan), might be necessary depending on initial findings. These tests help pinpoint the source of bleeding, which could range from kidney stones to bladder cancer. Do not delay seeking professional medical help.
Additional diagnostic tests
Depending on the initial results, your doctor may order additional blood tests to evaluate your kidney function and look for other underlying health conditions. These tests provide a broader picture of your overall health, helping to contextualize the findings from the urine analysis and imaging studies. Accurate diagnosis and timely intervention are crucial for managing hematuria effectively and addressing potential underlying causes.
When to Seek Medical Attention: Risk Factors and Complications
Notice blood in your urine after starting Lasix? Contact your doctor immediately. This isn’t always cause for alarm, but warrants prompt evaluation.
Risk Factors Increasing the Likelihood of Complications: Pre-existing kidney disease significantly increases the risk of Lasix-induced complications. Older adults, those with heart failure, and individuals with a history of dehydration are also more vulnerable. Concurrent use of certain medications, like NSAIDs, can also heighten the risk.
Specific complications requiring immediate medical attention include:
- Severe dehydration: Symptoms include dizziness, lightheadedness, and excessive thirst. Severe dehydration can lead to serious complications.
- Low potassium levels (hypokalemia): Muscle weakness, cramps, and irregular heartbeat are potential signs. Hypokalemia can be life-threatening.
- Kidney damage: Persistent blood in urine, along with decreased urine output or pain, could indicate kidney damage. Seek immediate care.
- Allergic reactions: Rash, itching, swelling, and difficulty breathing require immediate emergency medical attention.
When to Go to the Emergency Room: Seek immediate emergency care if you experience sudden, severe pain in your lower back or side, along with blood in your urine, or any combination of the above symptoms. Don’t hesitate to seek emergency assistance if you’re experiencing breathing difficulties or severe allergic reactions.
Regular monitoring of your blood pressure and kidney function during Lasix treatment is recommended. Open communication with your doctor about any concerns, however minor, is crucial for managing potential risks effectively.
Managing Lasix-Related Hematuria: Treatment and Prevention
Discontinue Lasix if hematuria develops. Your doctor will assess the severity and determine the best course of action.
Hydration is key. Increase your daily fluid intake to help flush out your system. Aim for at least eight glasses of water unless your doctor advises otherwise.
Monitor your urine. Note the color and frequency. Report any changes to your physician immediately. Consistent monitoring helps early detection of problems.
Dietary adjustments may be necessary. Reduce intake of foods and drinks known to irritate the urinary tract, such as acidic juices and spicy foods. Your doctor can provide personalized guidance.
Consider alternative diuretics. Your doctor might suggest a different diuretic if Lasix is deemed the cause of the hematuria. Discuss other options available to you.
Regular check-ups are crucial. Schedule follow-up appointments as advised to track your progress and address any concerns. Consistent monitoring provides the best chance of managing hematuria.
Blood tests may be ordered. These tests help determine the cause of the bleeding and guide treatment decisions. Follow your doctor’s recommendations for any required blood work.
Underlying conditions must be addressed. Hematuria can sometimes stem from other health problems. Your physician will conduct necessary tests to rule out other potential causes.