Book a doctor’s appointment online; it’s faster and often more convenient than calling. Many clinics now offer this service, saving you valuable time. This simple action can significantly improve your access to healthcare.
Canada boasts a publicly funded healthcare system covering medically necessary services. However, wait times for specialists can vary regionally. Proactive health management, such as regular check-ups and preventative screenings, can mitigate potential delays and ensure your health remains a priority.
Consider supplemental health insurance to cover services not included in the public system, such as dental, vision, and prescription drugs. These private plans offer additional protection and can help you manage out-of-pocket expenses. Compare plans carefully to find the best fit for your needs and budget.
Provincial healthcare systems vary slightly. Understanding your province’s specific programs and resources is key. Use the provincial government’s health websites to access detailed information about available services and eligibility requirements. Knowing your rights and responsibilities allows you to actively participate in managing your health.
- Canadian Health
- Prescription Drug Coverage
- Seeking Medical Attention
- Mental Health Services
- Preventive Care
- Additional Resources
- Funding the Canadian Healthcare System: Tax Dollars at Work
- Accessing Healthcare: Navigating the System for Residents and Tourists
- Physician Availability and Wait Times: Understanding Regional Differences
- Prescription Drugs and Coverage: A Look at Public and Private Options
- Emergency Care in Canada: Knowing Your Rights and Options
- Mental Health Services in Canada: Accessing Support and Resources
- Alternative and Complementary Therapies: Their Role in the Canadian Healthcare Landscape
Canadian Health
Consider a Provincial Health Card for seamless access to publicly funded healthcare. This card provides coverage for medically necessary services like doctor visits, hospital stays, and some prescription drugs. Eligibility depends on residency status and provincial regulations; check your province’s website for specific details.
Prescription Drug Coverage
Provincial drug plans offer varying degrees of coverage, often dependent on age and income. Many Canadians supplement this with private insurance through their employers or individual plans. Compare plans carefully, focusing on specific medications you need and their coverage levels. Expect cost-sharing even with provincial coverage.
Seeking Medical Attention
For non-emergency situations, Family Doctors provide primary care. Booking appointments usually requires some waiting; consider registering with a clinic early to secure faster access. Walk-in clinics offer same-day appointments for minor illnesses and injuries. Emergency rooms handle urgent and life-threatening situations; however, expect potentially longer wait times.
Mental Health Services
Access to mental healthcare varies across provinces. Some provinces offer publicly funded counseling and therapy services, while others rely more on a combination of public and private options. Explore services offered by your province’s health authority. Online resources and helplines are available nationwide, providing immediate support and referrals.
Preventive Care
Regular check-ups with your doctor, along with screenings for conditions like cancer and diabetes, are crucial. Take advantage of preventative services to maintain optimal health. Many provinces offer free or subsidized screenings.
Additional Resources
Health Canada’s website provides comprehensive information on national health initiatives and programs. Your provincial health authority’s site offers details on local healthcare services and regulations.
Funding the Canadian Healthcare System: Tax Dollars at Work
Canadians fund their healthcare system primarily through general taxation. Federal and provincial governments share responsibility, with the federal government contributing approximately 22% of total health spending in 2022, while provinces and territories cover the remaining 78%. This translates to a significant portion of individual income taxes directly supporting healthcare services.
Provincial governments levy various taxes, including income taxes, sales taxes and health premiums (in some provinces), to finance the majority of their healthcare budgets. These funds cover physician and hospital services, prescription drug coverage (which varies by province), and other healthcare programs. For example, Ontario’s health budget in 2022 exceeded $70 billion.
Transparency remains a key area for improvement. While governments publish annual reports detailing healthcare expenditures, making this information easily accessible and understandable for the average citizen is crucial. Clearer visualizations of how tax dollars are allocated across different healthcare sectors – hospitals, primary care, mental health, etc. – would significantly improve public understanding and accountability.
Optimizing funding allocation necessitates ongoing assessment and strategic planning. Investing in preventative care, for example, may ultimately reduce long-term healthcare costs. Regular independent audits of healthcare spending, coupled with publicly available data analysis, could identify areas for cost savings and efficiency improvements. Furthermore, exploration of alternative funding models, including targeted taxes or increased private sector involvement for certain services, deserves careful evaluation.
Public engagement is paramount. Open forums and transparent discussions about healthcare funding, challenges, and potential solutions can foster public trust and contribute to informed policy decisions. Active participation from healthcare professionals, policymakers, and citizens ensures that the system remains responsive to evolving needs and resource constraints.
Accessing Healthcare: Navigating the System for Residents and Tourists
Residents access healthcare through their provincial or territorial health insurance plan. Register with your province or territory upon arrival to obtain a health card, providing proof of residency. This card grants access to most medically necessary services, including doctor visits, hospital stays, and some prescription drugs.
Tourists should carry comprehensive travel insurance. This insurance typically covers medical emergencies and hospitalizations. While some emergency services are available without upfront payment, expect to present your insurance details for reimbursement later. Always keep your insurance information readily available.
For non-emergency situations, finding a doctor requires research. Use online directories or ask your hotel for recommendations. Booking appointments is common, so plan accordingly. Expect potential wait times, especially for specialists.
| Service | Residents | Tourists |
|---|---|---|
| Doctor Visits | Covered by provincial/territorial plan | Covered by travel insurance; expect costs upfront |
| Hospital Stays | Covered by provincial/territorial plan | Covered by travel insurance; expect costs upfront |
| Prescription Drugs | Partial coverage varies by province/territory | Covered by travel insurance; expect costs upfront |
| Emergency Services | Covered by provincial/territorial plan | Emergency services provided, billing handled later via insurance |
Pharmacies dispense prescription medications. Present your prescription and health card (for residents) or insurance information (for tourists). Over-the-counter medications are readily available at pharmacies and grocery stores.
Dial 911 for emergencies. This number connects you to emergency medical services throughout Canada. For non-emergencies, use online resources to find the appropriate healthcare provider.
Physician Availability and Wait Times: Understanding Regional Differences
Canadians experience vastly different wait times for physician appointments, depending on their location. Rural areas generally face longer waits than urban centers.
- Rural Ontario: Expect average wait times of 2-4 weeks for a family doctor appointment and significantly longer for specialists. Consider telehealth options or travelling to nearby urban centers for faster access.
- Urban British Columbia: Wait times vary widely. Larger cities like Vancouver and Victoria may offer quicker access to specialists (though still potentially lengthy, averaging 4-8 weeks), compared to smaller communities, where waits can extend several months. Pre-booking appointments is crucial.
- Quebec City: While access to family physicians is generally good, specialized care, such as cardiology or oncology, frequently involves waiting periods exceeding 6 weeks. Consider registering with a family clinic ahead of time to establish a relationship and expedite future requests.
These disparities stem from several factors:
- Physician Density: Rural areas often have a far lower ratio of physicians per capita than urban areas.
- Physician Specialization: The availability of specialists is significantly lower outside of major cities.
- Infrastructure: Remote locations may lack the necessary infrastructure to support telehealth or efficient referral systems.
- Population demographics: An aging population in some areas contributes to increased demand.
To mitigate long waits:
- Register with a family doctor early: This provides ongoing care and a faster route to specialist referrals when needed.
- Utilize telehealth services: Many provinces offer virtual consultations for non-emergency situations.
- Explore walk-in clinics: For non-urgent issues, walk-in clinics provide more immediate access to physicians.
- Consider private clinics: While not covered by provincial health insurance, private clinics may offer faster appointment times (at a cost).
Provincial health authorities regularly publish data on wait times. Consult their websites for the most current information specific to your region. Proactive planning is key to receiving timely medical care.
Prescription Drugs and Coverage: A Look at Public and Private Options
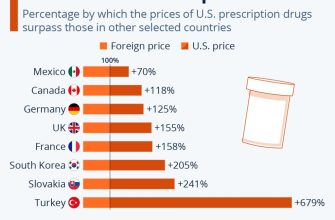
Canadians face varied prescription drug coverage depending on their province and personal circumstances. Public plans offer some protection, but significant gaps remain.
Provincial drug plans typically cover medications for seniors and low-income individuals. Coverage varies widely; some provinces offer broader benefits than others. For example, Ontario’s drug plan has a larger formulary than some Atlantic provinces. Check your provincial government’s website for details on eligibility and covered drugs.
- Consider your province’s formulary: This list dictates which medications are covered. If your medication isn’t listed, you’ll likely need private insurance or pay out-of-pocket.
- Explore options for low-income individuals: Many provinces offer subsidized or free prescription drug programs for those meeting specific income requirements.
- Check your employer’s benefits: Many employers provide supplemental drug plans, reducing your out-of-pocket expenses. Review your employee handbook for details.
Private insurance provides another avenue for prescription drug coverage. These plans often offer broader coverage than public plans, including brand-name drugs and specialty medications. The cost varies significantly depending on the plan’s features and your insurer.
- Compare plans carefully: Consider coverage levels, premiums, and deductibles before selecting a private plan. Use online comparison tools to help.
- Assess your needs: Determine what medications you regularly need and whether a plan offers sufficient coverage for those drugs.
- Factor in pre-existing conditions: Some pre-existing conditions might affect your eligibility or the cost of a private plan.
Paying for prescriptions without insurance can be expensive. Generic alternatives frequently cost less than brand-name medications. Ask your pharmacist about affordable options. Consider using a discount drug card if you don’t have insurance coverage. Many pharmacies offer these cards, potentially reducing your costs.
Emergency Care in Canada: Knowing Your Rights and Options
Dial 911 immediately for life-threatening emergencies. Paramedics will provide initial assessment and transport to the nearest appropriate hospital.
You have the right to receive emergency medical care regardless of your insurance status or ability to pay. Hospitals must provide necessary treatment, even if you can’t afford it. Follow-up care might require a different payment process.
Provincial health insurance plans cover emergency services. However, you might still incur costs for things like ambulance transportation (depending on your province) or certain medications received in the emergency room. Check your provincial plan details for specifics.
Clearly communicate your symptoms and medical history to medical professionals. This helps ensure you get the most accurate diagnosis and treatment. Bring a list of current medications if possible.
If you are dissatisfied with the care you received, you can file a complaint with your provincial health authority. Each province has its own process for handling complaints. Information about these processes is generally available online through the provincial health ministry website.
For non-emergency health concerns, consider using telehealth services or contacting your family doctor. These options might be faster and more convenient than visiting an emergency room for less urgent issues.
Understand that wait times in emergency rooms can vary significantly depending on the hospital and the time of day. Be prepared for potential delays. Emergency departments prioritize patients based on the severity of their condition.
Mental Health Services in Canada: Accessing Support and Resources
Need help? Contact your family doctor. They can provide initial assessments, prescribe medication if necessary, and refer you to specialists like psychiatrists or psychologists.
For immediate crisis support, dial 911 or visit your nearest emergency room. Alternatively, you can contact the Crisis Services Canada hotline at 1-833-456-4566 for 24/7 support.
Many provinces offer online mental health resources and virtual therapy sessions. Check your provincial health authority website for specific programs and eligibility criteria. For example, Ontario’s website provides details on various mental health services, including access to virtual care.
Consider exploring community-based mental health organizations. Many non-profit groups offer support groups, workshops, and individual therapy, often at lower costs than private practitioners. A quick online search for “mental health services [your city/province]” will yield relevant results.
If you have a workplace, inquire about employee assistance programs (EAPs). Many companies provide access to counselling and other mental health resources as part of their benefits package.
Remember, accessing mental health support is a sign of strength, not weakness. Take proactive steps to improve your wellbeing. Don’t hesitate to reach out for help when you need it. Your health matters.
Alternative and Complementary Therapies: Their Role in the Canadian Healthcare Landscape
Canadians increasingly integrate alternative and complementary therapies (ACTs) into their healthcare routines. Acupuncture, chiropractic care, and massage therapy are among the most popular choices, often used alongside conventional medicine.
Government regulation varies across provinces and territories. For instance, some provinces license and regulate practitioners of acupuncture, while others do not. Always verify a practitioner’s credentials and licensing before seeking treatment.
Insurance coverage for ACTs differs significantly. While some plans cover certain modalities, like physiotherapy, others may offer limited or no coverage for ACTs. Contact your insurance provider directly to understand your specific coverage.
| Therapy | Common Uses | Provincial Regulation (Example: Ontario) |
|---|---|---|
| Acupuncture | Pain management, nausea relief | Regulated by the College of Traditional Chinese Medicine Practitioners and Acupuncturists of Ontario |
| Chiropractic Care | Musculoskeletal issues, pain relief | Regulated by the College of Chiropractors of Ontario |
| Massage Therapy | Pain relief, stress reduction | Regulated by the College of Massage Therapists of Ontario |
Research into the efficacy of various ACTs is ongoing. While some treatments show promise, further studies are needed to establish definitive conclusions about their benefits in various conditions. Discuss the potential risks and benefits of any ACT with your doctor before beginning treatment.
Remember, ACTs should complement, not replace, conventional medical care for serious illnesses. Always consult your physician for diagnosis and treatment of health problems. A collaborative approach, integrating both conventional and complementary therapies, often provides the best patient outcomes.